February 2006: Sgt. Jon Trevino shot his estranged wife,
Carol Trevino, five times, the last time in the head. Then he shot himself. The
couple’s nine year old son sat in bed and watched his father kill his mother in
cold blood (Alvarez & Sontag, 2008).
September 2008: 19 year old Jacqwelyn Joann Villagomez was
beaten and choked to death by her boyfriend, John Wylie Needham. Needham was a
25 year old Iraqi veteran who suffered combat injuries. His family reported
that he returned home with severe mental problems, pain from the shrapnel in
his legs and back and struggled with nightmares that left him screaming
(Esquivel and Hanley, 2008).
August 2008: Jessie Bratcher, Iraqi war veteran and National
Guardsman, shot (10 times) and killed Jose Ceja Medina, the man he believed had
raped his girlfriend. It was later learned that Bratcher's Humvee was hit by a
roadside bomb in Iraq in 2005 but the team reported no injuries, though
Bratcher and his team leader both had headaches. It was not until 2008 that Bratcher’s
recurring anxiety, depression and mood swings were classified as a traumatic
brain injury from the blast -- symptoms which overlap and mimic post-traumatic
stress disorder (Sullivan, 2009).
April 2009: Less than a year after returning from combat in
Iraq, Nick Horner shot and killed Raymond Williams, a retired 64 year old in
Pennsylvania. Horner also killed a teenager and wounded a woman at a store in
the same town. Horner did not know any of these victims. After he returned from
Iraq, Horner was a different person, his mother said. He barely left his home
and, oftentimes, “his wife would find him crying in the corner of the basement”
(Lawrence & Rizzo, 2012).
How many more of these stories will it take before the
effects of war on our veterans are taken seriously?
(Lee, 2013)
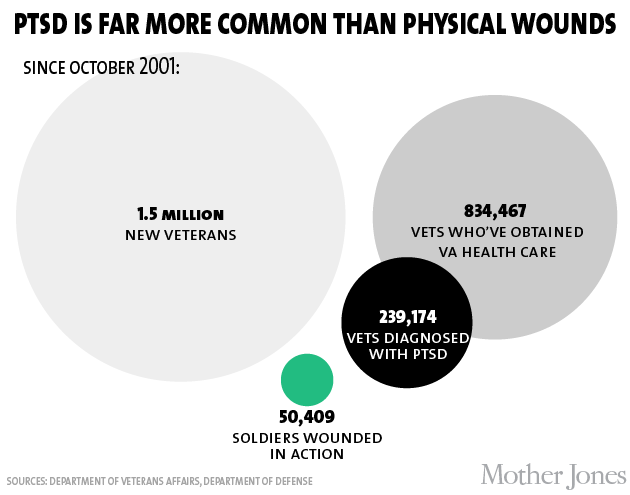
Nearly 20 percent of all Operation Enduring Freedom and
Operation Iraqi Freedom veterans screened positive for Post-Traumatic Stress
Disorder (PTSD) in 2008 (Banai, Maxwell, O’Neal, & Gallagher, 2011). The
actual rate of veterans with PTSD is probably much higher. The symptoms of
PTSD, according to the VA, are reliving the event, avoiding situations
reminiscent of the event, feeling numb, and hyperarousal. Hyperarousal is the
feeling jittery and always being on alert and on the lookout for danger (PTSD)
(National Center for PTSD, 2013). The effects of hyperarousal have been blamed
for the high rates of violence among veterans. Service members with PTSD (who
sought therapy) found that 80 percent committed a violent act within the past
year. This is six times higher than the civilian population (Banai et al., 2011).
Iraq and Afghanistan veterans who struggle with anger are twice as likely as
other vets to be arrested for crimes, according to the Journal of Consulting
and Clinical Psychology, which published a study last year (Fantz, 2013). In 2009, at least 122 soldiers who served in
Iraq and Afghanistan had been charged in or convicted of a killing. A 2009 Army
study of 11 killings committed by members of Fort Carson, Colorado concluded
that those soldiers were affected “by combat in Iraq, alcohol and drug abuse,
previous mental health issues and PTSD” (Sullivan, 2009).
(Lee, 2013)
The mental instability, anxiety and anger associated with
PTSD are destructive for most military families. PTSD increases the chance of
family violence, divorce and drug and alcohol abuse. A veteran suffering from PTSD may be unable to
fulfill his or her roles as a parent, spouse or contributing member of society.
This puts a considerable amount of strain on the family. Despite the fatal
effects of PTSD, most military families do not seek treatment for PTSD because
of the stigma associated with mental disorders (Banai et al., 2011). Unfortunately, treatment for this condition
is not readily available for those veterans willing to reach out for help.
Take the story of Jessie Bratcher (the Vet who killed the
alleged rapist of his girlfriend): After returning home from war, his grandfather heard him at night, "hollering, a bunch
of mumbo jumbo, like a frightened child” and Jessie continuously asked for guns
(Sullivan, 2009). Bratcher
went to the VA for help because he was unable to work but his attempt to
collect benefits was denied. The VA decided that his PTSD symptoms were
"too mild." Though
it's widely treated, the number of Iraq and Afghanistan vets compensated for PTSD
is fewer than 2 percent of veterans receiving benefits. “Nationally, almost 4
percent of World War II and Korean vets and 7 percent of Vietnam vets receive
money for PTSD” (Sullivan, 2009). Not
only is compensation for symptoms of PTSD difficult for vets to receive, but
proper counseling is also scarce. There are not a high number of therapists who
are experts in PTSD and who understand how to really help the victims. Vets may
not want to talk to a civilian who has no idea about the terror he/ she has
gone through. More research needs to be put into different strategies to help
these vets.
(Lee, 2013)
Sergeant Trevino had been treated twice for mental health
problems before the war: once for serious depression as his first marriage
crumbled, and then again for post-traumatic stress disorder stemming from the
childhood sexual abuse and also marital problems with his new wife, Carol. He
was counseled and treated with medication both times. The Air Force was fully
aware of the instability of Trevino’s mental state yet military doctors
certified that he could handle the job. The Air Force considers the stress
disorder to be treatable and is willing to deploy an airman with a history of
it. When Trevino returned home from his deployment, Trevino began taking a mix of
antidepressants and therapy prescribed by the military. However, the damage had
already been done (Alvarez & Sontag, 2008). The Air Force, the institution
that Trevino had dedicated his life and loyalty to, had greatly betrayed him
and his family by failing to safeguard the health of their soldier before
anything else. Unfortunately, this is not a common occurrence since the need
for soldiers overseas is greater than our actual numbers.
(Lee, 2013)
The reality of PTSD within our military population is
overwhelming. Not only does PTSD
increase the likelihood of violence for families and society, it also increases
the incidence of self-inflicted violence. These images give us a clear picture
of the effect of PTSD on the well-being of our nation’s heroes.
(Lee, 2013)
I hope that within the next few years we will see an
increase in PTSD specialists and funding for rehabilitation programs. Although
not all returning vets have PTSD, a significant amount does and they need our
attention and support.
Questions:
1.
Why would military families not want to seek out
treatment for PTSD?
2.
Should universities offer concentrations or
specializations in PTSD therapy?
*If you enjoy watching those surprise coming home videos,
here is the video of when one of my best friends surprised us on Christmas last
year. Enjoy!*
Leandra Furtado
References:
Alvarez, L. &
Sontag, D. (February 2008). When Strains on Military Families Turn Deadly. New York Times. Retrieved from http://www.nytimes.com/2008/02/15/us/15vets.html?pagewanted=all&_r=0
Banai, M.,
Maxwell, B., O’Neal, J., Gallagher, M. (2011, December ). Unsung Heroes:
Military Families after 10 Years of War. In IAVA
Issue Report: December 2011. Retrieved from https://my.lesley.edu/courses/1/13-SP.CSOCL.2402.01.73885/content/_1124354_1/Unsung_Heroes.pdf
Esquivel
P. & and Hanley, C. (September 2008). 'Mentally unstable' Iraq veteran
arrested in death of girlfriend, 19. Los Angeles Times. Retrieved from http://www.latimes.com/news/local/la-me-beating3-2008sep03,0,6026971.story
Fantz,
A. (February 1013). Sniper Killing Aftermath: 5 Things to Know about PTSD. CNN Health. Retrieved from http://www.cnn.com/2013/02/05/health/ptsd-five-things
Lawrence,
C. & Rizzo, J. (May 2012). Under Fire: Wartime Stress as a Defense for
Murder. CNN Justice. Retrieved from http://www.cnn.com/2012/05/05/justice/ptsd-murder-defense
Lee, J.(January 2013). Charts: Suicide, PTSD and the Psychological Toll on America's Vets. Mother Jones. Retrieved from http://www.motherjones.com/politics/2013/01/charts-us-veterans-ptsd-war-iraq-afghanistan
Sullivan,
J. (October 2009). Trauma in Iraq leads to drama in Oregon. The Oreganian.
Retrieved from http://www.oregonlive.com/news/index.ssf/2009/10/post_25.html.
National
Center for PTSD. (2013). What is PTSD? United
States Department of Veteran Affairs. Retrieved from http://www.ptsd.va.gov/public/pages/what-is-ptsd.asp
Leandra Furtado








No comments:
Post a Comment